Introduction
I have been wanting to write an article about constipation and the role of fiber for a while, but yesterday I saw a cartoon drawn by Glenn McCoy that was the final motivation.
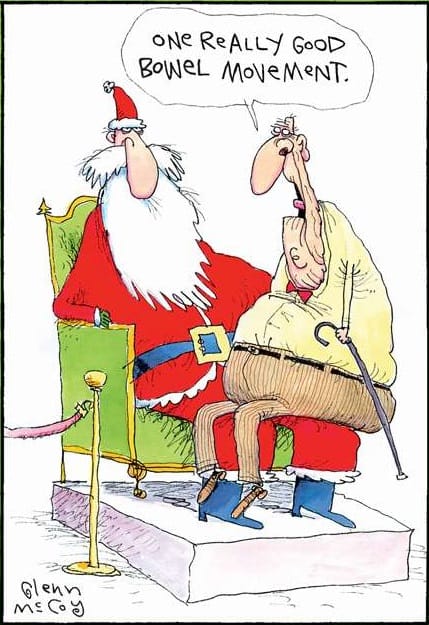
(posted with written permission from Glenn McCoy)
The old song “All I Want for Christmas (is my two front teeth)” may apply to children, but many adults can relate to this cartoon! The number of people I see in my practice who complain about constipation is ~1/4 to 1/3 — and I know this because one of the questions I routinely ask during an assessment is ‘how many times per day, or per week do you poop’, and I ask them to describe their poop (soft, hard, like bunny poop, floats, etc.). Yes, really! I ask about pooping because it is important, and I also ask about sleep, because that is important too.
Epidemiology and Prevalence of Chronic Constipation
The percentage of adults that I see who struggle with chronic constipation is ~15- 20%, which fits what is seen in the literature. Based on self-report or using the Rome IV criteria, constipation is a problem for between 2% and 27% of the population, with an average of 15% [1].
Rome IV Diagnostic Criteria for Functional Constipation
Constipation, as defined by the Rome IV criteria, needs to meet at least two of the following symptoms over the previous three months [2]. Put in common language, those symptoms are;
- having fewer than 3 bowel movements (BMs) per week without taking something to “go” (i.e., having spontaneous bowel movements)
- pushing or straining for at least 1/4 of BM attempts
- lumpy or hard stools for at least 1/4 of BM attempts
- a feeling of something blocking the anus or rectum for at least 1/4 of BM attempts
- feeling of still needing to poop after pooping (i.e., incomplete defecation) for at least 1/4 of BM attempts
- physically positioning differently or using manual manipulation for at least 1/4 of BM attempts
It is important to note that the Rome IV criteria also state that to meet the criteria for constipation, one must NOT also meet the criteria for Irritable Bowel Syndrome (IBS). These are different disorders. While people with IBS may have constipation, they may also have diarrhea, or may have alternating symptoms of constipation and diarrhea. IBS’ main symptom is abdominal pain related to bowel movements.
Distinguishing Functional Disorders from Structural Disease
The Rome IV criteria for IBS [3] require having recurring symptoms of abdominal pain at least one day per week during the previous three months and associated with 2 or 3 of the following;
- defecation (pooping)
- a change in the number of times one poops (stool frequency)
- a change in stool form or appearance
Chronic constipation and IBS are both referred to as “functional gastrointestinal diseases” (FGIDs). These are common disorders that are ongoing and recurring and whose symptoms are not caused by some underlying disease or structural abnormality of the GI tract [4]. These are different than something like diverticulosis, which is a pouch that forms in the large intestine and which requires monitoring the amount of fiber one takes in to avoid constipation.
[NOTE: December 24, 2021: I think a better term for these conditions is “functional gastrointestinal disorders” because these do not have a structural cause. A physician I know described it this way: “A rule of thumb is that a disease is something a pathologist can see.”]
There are no tests for constipation or IBS. They are diagnosed based on symptoms or function.
The Insoluble vs. Soluble Fiber Paradigm
Most people who are diagnosed with “constipation*” are told by their doctors to “eat more fiber and drink more water”.
A diagnosis of “idiopathic constipation” means that the constipation occurred spontaneously on its own, and has no known cause. “Chronic idiopathic constipation” is chronic constipation that has no known cause.
Most people who come to me think of fiber as “roughage” that includes things such as whole, unrefined grains, wheat bran, oat husks, and the like. Horse food! The term “insoluble fiber” is used to describe these because these fibers do not dissolve in water. Insoluble fiber is not digested, so it just adds “bulk” to the stools.
Soluble fiber dissolves in water and, as a result, creates a gel-like texture in the intestine when mixed with the water contained in food or in beverages. This is where the “drink more water” advice comes in — it is for the soluble fiber to form that gel. Soluble fiber helps slow down digestion, enabling people to feel fuller longer, and helps form a soft, bulky stool. While people don’t usually think of these types of foods as “high in fiber”, foods high in soluble fiber include onions, chicory root, Jerusalem artichoke, oats, apples, strawberries, psyllium husk, and some legumes (or pulses).
Clinical Outcomes of Fiber Reduction in Idiopathic Constipation
The six-million-dollar question is whether increasing dietary fiber actually improves constipation. In fact, a ground-breaking study from 2012 found the exact opposite! Symptoms of ‘idiopathic constipation’ were significantly reduced when people in the study lowered, or even stopped their high intake of dietary fiber [5]. This made sense to the researchers, who explained that ‘since increasing dietary fiber increases the volume and bulk of the stools, in patients where there is already difficulty in passing large stools, it is illogical to actually expect that bigger or more feces will ameliorate (i.e., improve) this problem.’ Of interest, people in the study who went on to eat the least amount of fiber in their diet had the greatest reduction in symptoms, and those who went back to eating a high fiber diet also began to experience their previous symptoms of constipation, in proportion to the amount of fiber they ate in their diet [5]!
So, if increasing fiber intake is not the answer to maintaining ‘regularity’ in our colon, what is?
Soluble Fiber and the Gut Microbiome
Soluble fiber helps feed the healthy bacteria that live in our bowel (large intestine) called the ‘gut microbiome’ or ‘gut flora’. We are in a mutually beneficial (symbiotic) relationship with them, which means they benefit us, and we benefit them. What we eat feeds them, and in turn, they produce by-products that are helpful for us.
Post Publication Update: (December 24, 2021) The gut microbiome uses soluble fiber as “food” and, in return, produces three short-chain fatty acids: acetate, butyrate, and propionate [10]. The butyrate produced by the gut microbiota is the main “food” (energy source) of the cells of our intestine — especially the colonocytes (cells in the lumen of our colon) [11]. Our gut microbiome feeds on the fiber in our food and produce short chain fatty acids in return, and in turn, these short-chain fatty acids feed the cells of our colon! These short-chain fatty acids that are fermented by our gut microbiome are what maintain the homeostasis (balance) of our intestines [12].
Ketogenic Metabolism and Intestinal Health
People who eat a very low-carbohydrate (ketogenic) diet produce a closely-related short chain fatty acid known as β-hydroxybutyrate, which can be measured in the blood. Recent studies have found that β (beta)-hydroxybutyrate acts very similarly to butyrate [9] and β (beta)-hydroxybutyrate also feeds the cells of the colon, as well as the cells of the small intestine. The main difference is that when the cells of the intestine are fed β-hydroxybutyrate via the capillaries of the blood, this is thought to be less irritating to the cells of the colon than when they feed on butyrate produced by the gut microbiota.
[Many thanks to Dr. Lance de Foa of Wawa, Ontario, for bringing the above information to my attention.]
Pathological Impact of Simple Sugars on Mucosal Barriers
Something else that is very important to note is that the gut microbiome can also be adversely affected by the type of carbohydrate we eat.
A study published in late 2020 documented how simple sugars in the diet can induce colitis, an inflammatory bowel disease [6] in mice. The study found that when researchers fed the mice simple sugars such as fructose (fruit sugar), sucrose, (table sugar made up of glucose and fructose) and glucose, the high simple sugar diet damaged the protective mucus layer of the colon (large intestine) and increased the number of specific bacteria — especially Akkermansia muciniphila and Bacteroides fragilis which break down the mucus that lines and protects the colon. When the mice were fed a 10% glucose solution for seven days (chosen because soft drinks contain ~15% sugar) and were then given a 2.5% dextran sulfate sodium (DSS) which is known to induce colitis, the mice that had been fed the glucose had extreme sensitivity to DSS treatment and suffered from aggressive colitis, bloody diarrhea and rapid loss of nearly 20% of their body weight. When the researchers looked at the glucose-treated mice three days after giving them the DSS, they found that their colons were shorter than the colons of the control mice that were not fed the glucose, and that the glucose-fed mice had many of the symptoms of colitis, including loss of epithelial crypts, inflammation, and ulceration [5].
The control mice remained healthy, with stable weight [5]. Both the glucose-treated mice and the mice that were not given glucose ate comparable amounts of food and water during DSS administration — which implied that the colitis susceptibility of glucose-fed mice was not due to any increase in DSS intake.
A second arm of the study found that a high sugar intake alone had a similar effect as the DSS in mice that were genetically susceptible to colitis.
Ketogenic Diet and Microbial Regulation
A different small randomized, double-blind crossover study pilot study from 2020 [7] looked at the effect of a very low-carbohydrate (ketogenic) diet on the population of the gut fungi and microbiome and found that a very low-carbohydrate diet more positively affected the gut than the diet used in the control group, the American Heart Association Diet. What was notable was a significant reduction in the proportion of Candida yeast, which is implicated in various gut-related diseases, including inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, as well as gut inflammation.
In my practice, I describe the relationship between us (as the host) and our microbiome using the analogy of “feeding turtles”. If we think of our intestines as a terrarium with two types of turtles — “good turtles” and “bad turtles”, if we only feed the good turtles, and don’t feed the bad turtles, the bad ones will die off, and the good ones will get stronger and proliferate. If we feed our “good” microbiome and starve out the “bad” ones, we will have a healthier gut. While the above studies are preliminary, it makes sense that if we reduce simple carbohydrate intake in the diet (sucrose, lactose, and glucose), we won’t be feeding the “bad turtles”, which means they will be reduced or even die off. If we eat foods high in soluble fibers that feed the “good turtles”, they will get stronger and proliferate.
Therapeutic Efficacy of Partially Hydrolyzed Guar Gum (PHGG)
In addition to insoluble fiber and soluble fiber, there is another class of fibers, which are water-soluble, non-gelling fibers, including one called partially hydrolyzed guar gum (PHGG). This fiber plays an important role in alleviating symptoms of constipation or diarrhea because it is not probiotic, but a prebiotic. It is like “turtle food” for the “good turtles”. Partially hydrolyzed guar gum (PHGG) has been shown in clinical trials to both decrease symptoms in constipation-predominant IBS and diarrhea-predominant type IBS, as well as decrease the hallmark symptom of abdominal pain [8], and works very well to alleviate symptoms of chronic constipation.
Putting it Into Practice
For those who want to know which foods are high in non-soluble fiber, these include red cargo rice (4 g fiber per 1/2 cup), or wholegrain brown basmati rice, such as Tilda® brand (4g fiber per 1/2 cup), and wholegrain breads made with whole and cracked wheat berries, or whole and cracked rye berries. Wholegrain breads are not the same as “brown bread” or “whole wheat bread”, but the type of bread one would find in a European bakery, a natural food store, or in a regular supermarket imported from Germany (e.g., Mestemacher® brand). I describe them to clients as heavy enough that if you dropped them on your food, it might leave a bruise. In specific conditions or stages of conditions, it is recommended to limit these foods.
As for soluble fiber, legumes are a good source, and while they contain 15g of carbohydrate per 1/2 cu,p they also are good sources of protein (~7g per 1/2 cup). Black beans have 8.7 g of soluble fiber per 100 g, lentils have 7.3 g soluble fiber / 100g, chickpeas have 7 g soluble fiber / 100g, and kidney beans have 6.8 g soluble fiber / 100g.
Low carb vegetables that are a good source of soluble fiber include carrots (2.8 g/100g), beets (2.8g/100g), broccoli (2.6 g/100g), artichoke (5.4 g/100g), and Brussels sprouts (3.8g/100g) and fruit such as raspberries have 6.5g fiber / 100g, blackberries have 5.3 g fiber / 100g, and apples have 2.4g fiber/100g.
Even excellent sources of fat can come with soluble fiber, including avocado (6.7 g/100g) and Brazil nuts (8g / 100g).
The above foods can be incorporated into a wide range of dietary patterns — from omnivore, to vegetarian and pescatarian, Mediterranean, and low carb, and by also reducing intake of simple carbohydrates such as sucrose, lactose, and glucose, you can nourish yourself, as you feed your healthy microbiome.
More Info
Learn about me and the support I can provide to help you reduce chronic constipation. View my Comprehensive Dietary Package.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
Special Thanks
Special thanks to Glenn McCoy for permission to post his cartoon!
References
- Sanchez MI, Bercik P. Epidemiology and burden of chronic constipation. Can J Gastroenterol. 2011;25 Suppl B(Suppl B):11B-15B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3206558/]
- Drossman DA. Rome IV Diagnostic Questionnaires and Tables for Investigators and Clinicians. 1st ed. Raleigh, NC: Rome Foundation; 2016. [https://theromefoundation.org/rome-iv/rome-iv-educational-materials/rome-iv-diagnostic-questionnaires-and-tables/]
- Schmulson MJ, Drossman DA. What Is New in Rome IV. J Neurogastroenterol Motil. 2017;23(2):151-163. doi:10.5056/jnm16214 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5383110/]
- UNC Center for Functional GI & Motility Disorders. What is a Functional GI Disorder? 2017. [https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/What-Is-Functional-GI.pdf]
- Ho KS, Tan CY, Mohd Daud MA, Seow-Choen F. Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms. World J Gastroenterol. 2012;18(33):4593-4596. doi:10.3748/wjg.v18.i33.4593 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435786/]
- Khan S, Waliullah S, Godfrey V, et al. Dietary simple sugars alter microbial ecology in the gut and promote colitis in mice. Sci Transl Med. 2020;12(567):eaay6218. doi:10.1126/scitranslmed.aay6218 [https://www.science.org/doi/10.1126/scitranslmed.aay6218]
- Nagpal R, Neth B, Wang S, et al. Gut mycobiome and its interaction with diet, gut bacteria and alzheimer’s disease markers in subjects with mild cognitive impairment: A pilot study. EBioMedicine. 2020;59:102950. doi:10.1016/j.ebiom.2020.102950 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7452319/]
- Giannini EG, Mansi C, Dulbecco P, Savarino V. Role of partially hydrolyzed guar gum in the treatment of irritable bowel syndrome. Nutrition. 2006;22(3):334-342. doi:10.1016/j.nut.2005.10.003 [https://pubmed.ncbi.nlm.nih.gov/16413751/]
- Chriett S, Dąbek A, Wojtala M, et al. Prominent action of butyrate over β-hydroxybutyrate as histone deacetylase inhibitor, transcriptional modulator and anti-inflammatory molecule. Sci Rep. 2019;9(1):742. doi:10.1038/s41598-018-36941-9 [https://www.nature.com/articles/s41598-018-36941-9]
- Rios-Covian D, Ruas-Madiedo P, Margolles A, et al. Intestinal Short Chain Fatty Acids and their Link with Diet and Human Health. Front Microbiol. 2016;7:185. doi:10.3389/fmicb.2016.00185 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4756330/]
- Donohoe DR, Garge N, Zhang X, et al. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011;13(5):517-526. doi:10.1016/j.cmet.2011.02.018 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099420/]
- Venegas DP, De la Fuente MK, Landskron G, et al. Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Front Immunol. 2019;10:277. doi:10.3389/fimmu.2019.00277 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6413670/]

© 2025 BetterByDesign Nutrition Ltd.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
