Introduction
The role of diet in metabolic health is well-known, but many people do not realize that hormones, including those from the thyroid, impact that health significantly.
The Role of Thyroid Hormones
- from The Merck Manual of Medical Information (1997)
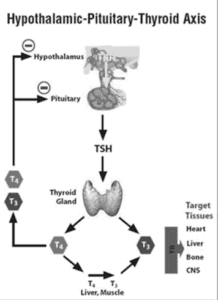
[Image of Hypothalamic-Pituitary-Thyroid Axis diagram]
The thyroid and the hormones it produces play an important role in metabolic health but it is a hormone from the pituitary gland called Thyroid Stimulating Hormone (TSH) that causes the thyroid gland to release the hormone thyroxine, also called free T4. Free T4 is the inactive form of thyroid hormone. Free T4 is activated (reduced) to free T3 (triiodothyronine), the active form of thyroid hormone.
Overt hypothyroidism is where TSH >10 mU/L, with normal or low free T4).
Subclinical hypothyroidism (SCH), which is where TSH is higher than the normal cutoffs (TSH >4 mU/L) but less than the criteria for overt hypothyroidism (TSH >10 mU/L), but with normal free T4.
Metabolic Changes due to Hypothyroidism
It has been well established for decades that people with overt (established) hypothyroidism experience several clinical changes that one might assume to be diet-related at first glance. For example, people with hypothyroidism have a decrease in red blood cells and experience different types of anemia, including the anemia of chronic disease. In addition, ten percent of people with hypothyroidism develop pernicious anemia, which is associated with vitamin B12 and folate (folic acid).
The slowing of metabolism associated with hypothyroidism also results in a decrease in cardiac (heart) output, which results in both slower heart rate and less ability for the heart to pump blood.
High Blood Pressure
The decreased ability of the heart to pump leads to increased resistance in the blood vessels, which results in increased blood pressure (hypertension).
In those who had normal blood pressure previous to developing hypothyroidism, blood pressure can rise as high as 150/100 mmHg. Hypothyroidism may increase it further for those previously diagnosed with high blood pressure.
It is not only diet that can contribute to high blood pressure but thyroid hormones (as well as other factors).
Weight Gain
Thyroid hormones act on every organ system in the body, but the thyroid is well-known for its role in energy metabolism. When someone has overt hypothyroidism, there is a slowing of metabolic processes, which results in symptoms such as fatigue, cold intolerance, constipation, and weight gain.
Weight gain is not only about diet or how much someone eats versus how much they burn off. It is also about the person’s metabolic rate, which can be impacted by several things, including decreased thyroid hormones.
High Cholesterol
It has long been known that those with overt hypothyroidism have high total cholesterol, high low-density lipoproteins (LDL) [14], and high triglycerides (TG) [15], which results from a decrease in the rate of cholesterol metabolism. While many assume that “high cholesterol” results from diet, such as the assumption it is related to eating too many eggs, thyroid hormones may also play a role.
Subclinical Hypothyroidism
It has been found that some people with subclinical hypothyroidism have high low-density lipoproteins (LDL) and triglycerides (TG) and low high-density lipoproteins (HDL) [16].
But it is not only high cholesterol that is also found in subclinical hypothyroidism. For example, a 2016 paper referred to above reported that previous studies found no significant difference in symptoms between people with subclinical hypothyroidism and those with overt hypothyroidism [9]. That is, all the symptoms associated with overt hypothyroidism are also seen in subclinical hypothyroidism. Therefore, to assume that high blood pressure, serum cholesterol, or blood sugar is solely the result of diet is to possibly overlook the role of the pancreas and/or the thyroid.
As I wrote about in the previous post, all too often, common symptoms of hypothyroidism are assumed to be normal signs of aging. Given the potentially serious consequencesof leaving hypothyroidism undiagnosed and untreated, people must be able to recognize these symptoms in themselves and loved ones.
Thyroid Hormones Affect Insulin Secretion of the Pancreas
Just as we cannot look at diet without considering the role of hormones such as insulin, we cannot look at pancreatic function in isolation from thyroid function.
As mentioned above, thyroid hormones influence every organ in the body, including the pancreas. It is now known that there are functional thyroid receptors in the pancreas that affect insulin secretion, and it is thought that thyroid hormones may play a role in the development of diabetes.
Diagnosis and Treatment
The most recent population-based study data from the US, with almost 26,000 adults aged 18 – 74 years, found 9.5% had TSH levels >5.1 mIU/L, with a higher prevalence in women and older adults. Among the 9.5% with elevated TSH, 74% had subclinical hypothyroidism (TSH 5.1 and 10 mIU/L), and 26% had overt hypothyroidism (TSH>10 mIU/L) [17].
Note (August 14, 2022): From a practical point of view, this study shows that almost 10% of adults have some form of hypothyroidism, with 7/10% being subclinical and 2½ % having clear hypothyroidism. Given its prevalence and significant risk of being undiagnosed, identifying symptoms and lab markers before it progresses is essential.
In British Columbia, a diagnosis of subclinical hypothyroidism is made at a TSH > 4 mIU/L, but treatment is only recommended when TSH is above 10 mIU/L [18]. This leaves those with a TSH >4 mIU/L but <10 mIU/L in the situation where they need to get much sicker before treatment is recommended.
The goal of treatment with thyroid hormone replacement is to reduce the patient’s serum TSH concentration into the normal reference range. Since the mean serum TSH for the general population is around 1.4 mIU/L, with 90% having serum TSH levels <3.0 mIU/L, many experts recommend a therapeutic TSH target ranging from 0.5 to 2.5 mIU/L in young and middle-aged patients [19] to 7.7 mIU/L in elderly people over the age of 80 years [20].
Studies with 10 to 20-year follow-up have reported that 33 to 55% of people with subclinical hypothyroidism progress to overt hypothyroidism [21,22,23]. This means that 1/3 to >1/2 of people with subclinical hypothyroidism will develop overt hypothyroidism within that period.
Most experts do not recommend treating people with a TSH > 10 mIU/L but with no symptoms (asymptomatic). However, since a meta-analysis of data from 1950-2010 found no increased risk of coronary heart disease in asymptomatic people with a TSH of 4.5 to 6.9 mIU/L, treating them is generally not recommended [24].
There is, however, an increased risk of coronary heart disease in those with a TSH of 7.0 to 9.9 mIU/L, so some experts recommend treating those with a TSH > 7.0 mIU/L whether or not they have symptoms [24]. Unfortunately, despite this elevated risk, individuals in British Columbia do not currently have access to treatment with a TSH < 10 mIU/L under the guidelines [18].
Final Thoughts…
Making recommendations on how someone should change their diet can’t be made in a vacuum, and it is for this reason that I evaluate a person’s lab test results in light of their medical history and enquire about family history of type 2 diabetes, heart disease, high cholesterol, blood pressure, thyroid disorders, and other conditions as part of the comprehensive assessment.
If I feel that it would be beneficial to have additional lab work, such as fasting insulin or thyroid-stimulating hormone (TSH), then I will request that their doctor requisition these tests. Often, when I provide the doctor with my clinical reasons for asking for them, they write the requisition; however, sometimes, they decline. If I don’t think it would not be a financial burden and that having the results will provide the client with a much better understanding of how their diet relates to their weight or health, I will discuss the option of obtaining the tests on a patient-pay basis.
NOTE (August 15, 2022): It is important to keep in mind that too little or too much thyroid hormone can have serious consequences.
Untreated or under-treated hypothyroidism can be serious as the body gets too little thyroid hormone. This can lead to a myxedema crisis, covered in this article.
Thyrotoxicosis can also be serious, and occurs when the body gets too much thyroid hormone. This can occur in untreated hyperthyroidism or by self-treating hypothyroidism, covered in this article.
If you suspect you may have hypothyroidism (or any other clinical condition), consult with your doctor.
More Info
As you can read about under the About Me tab, I will advocate for clients who have symptoms that may be consistent with hypothyroidism or subclinical hypothyroidism to obtain adequate testing to rule out a diagnosis or enable a doctor to make one. To learn more about the dedicated support I provide, please view my Hypothyroid Management Package here.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- Crofts C, Zinn C, Wheldon M, Schofield G. Identifying hyperinsulinaemia in the absence of impaired glucose tolerance: An examination of the Kraft database. Diabetes Research and Clinical Practice. 2016; 118:50-57. [https://doi.org/10.1016/j.diabres.2016.06.007]
- Pareek M, Bhatt DL, Nielsen ML, et al. Enhanced Predictive Capability of a 1-Hour Oral Glucose Tolerance Test: A Prospective Population-Based Cohort Study. Diabetes Care. 2018 Jan 1; 41(1):171–177. [https://doi.org/10.2337/dc17-1351]
- Sagesaka H, Sato Y, Someya Y, et al. Type 2 Diabetes: When Does It Start? Journal of the Endocrine Society. 2018 May 1; 2(5):476-484. [https://doi.org/10.1210/js.2018-00071]
- Government of British Columbia, Ministry of Health. Schedule of Fees for Laboratory Services – Outpatient, Payment Schedule. [Revised 2022 Apr 1]. [https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/medical-services-plan/laboratory_services_schedule_of_fees.pdf]
- BC Guidelines & Protocols Advisory Committee. Special Endocrine Testing: Indications and Appropriate Use – Insulin. Victoria (BC): Ministry of Health; [Published 2019 Jun 15, Accessed 2022 Aug 14]. [https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/special-endocrine-testing#Insulin]
- BC Guidelines & Protocols Advisory Committee. Special Endocrine Testing: Indications and Appropriate Use – C-peptide. Victoria (BC): Ministry of Health; [Published 2019 Jun 15, Accessed 2022 Aug 14]. [https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/special-endocrine-testing#C-peptide]
- Canadian Diabetes Association. The Burden of Out-of-Pocket Costs for Canadians with Diabetes. [Published 2011 Aug]. [https://www.diabetes.ca/DiabetesCanadaWebsite/media/Advocacy-and-Policy/Advocacy%20Reports/Burden_of_Out-of-Pocket_Costs_for_Canadians_with_Diabetes_Aug_2011.pdf]
- Statistics Canada. Table 11-10-0239-01 Income of individuals by age group, sex and income source, Canada, provinces and selected census metropolitan areas. [Accessed 2022 Aug 14]. [https://doi.org/10.25318/1110023901-eng]
- Javed Z, Sathyapalan T. Levothyroxine treatment of mild subclinical hypothyroidism: a review of potential risks and benefits. Therapeutic Advances in Endocrinology and Metabolism. 2016; 7(1):12-23. [https://doi.org/10.1177/2042018815616543]
- Danese MD, Ladenson PW, Meinert CL, Powe NR. Clinical review 115: effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. Journal of Clinical Endocrinology & Metabolism. 2000; 85(9):2993-3001. [https://doi.org/10.1210/jcem.85.9.6841]
- Caraccio N, Ferrannini E, Monzani F. Lipoprotein profile in subclinical hypothyroidism: response to levothyroxine replacement, a randomized placebo-controlled study. Journal of Clinical Endocrinology & Metabolism. 2002; 87(4):1533-1538. [https://doi.org/10.1210/jcem.87.4.8378]
- Nakajima Y, Yamada M, Akuzawa M, et al. Subclinical hypothyroidism and indices for metabolic syndrome in Japanese women: one-year follow-up study. Journal of Clinical Endocrinology & Metabolism. 2013; 98(9):3280-3287. [https://doi.org/10.1210/jc.2013-1399]
- Janovsky CCPS, Bittencourt MS, Goulart AC, et al. Unfavorable Triglyceride-rich Particle Profile in Subclinical Thyroid Disease: A Cross-sectional Analysis of ELSA-Brasil. Endocrinology. 2021 May 1; 162(5):bqab019. [https://doi.org/10.1210/endocr/bqab019]
- Lithell H, Boberg J, Hellsing K, et al. Serum lipoprotein and tissue lipoprotein-lipase activity in overt and subclinical hypothyroidism: the effect of substitution therapy. European Journal of Clinical Investigation. 1981; 11(1):3-10. [https://doi.org/10.1111/j.1365-2362.1981.tb01758.x]
- Nikkilä EA, Kekki M. Plasma triglyceride metabolism in thyroid disease. Journal of Clinical Investigation. 1972; 51(8):2103-2114. [https://doi.org/10.1172/JCI107019]
- Kung AW, Pang RW, Janus ED. Elevated serum lipoprotein(a) in subclinical hypothyroidism. Clinical Endocrinology. 1995 Oct; 43(4):445-449. [https://doi.org/10.1111/j.1365-2265.1995.tb02616.x]
- Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Archives of Internal Medicine. 2000 Feb 28; 160(4):526-534. [https://doi.org/10.1001/archinte.160.4.526]
- BC Guidelines & Protocols Advisory Committee. Thyroid Function Testing in the Diagnosis and Monitoring of Thyroid Function Disorder. Victoria (BC): Ministry of Health; 2018 Oct 24. [https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/thyroid-function-testing]
- Biondi B. The Normal TSH Reference Range: What Has Changed in the Last Decade? Journal of Clinical Endocrinology & Metabolism. 2013 Sep 1; 98(9):3584–3587. [https://doi.org/10.1210/jc.2013-2760]
- Surks MI, Hollowell JG. Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. Journal of Clinical Endocrinology & Metabolism. 2007 Dec 1; 92(12):4575–4582. [https://doi.org/10.1210/jc.2007-1499]
- Kabadi UM. ‘Subclinical hypothyroidism’. Natural course of the syndrome during a prolonged follow-up study. Archives of Internal Medicine. 1993 Apr 26; 153(8):957–961. [https://doi.org/10.1001/archinte.153.8.957]
- Vanderpump MP, Tunbridge WM, French JM, et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clinical Endocrinology. 1995 Jul; 43(1):55–68. [https://doi.org/10.1111/j.1365-2265.1995.tb01894.x]
- Mitrache C, Guglielmetti M, Huber P, Braverman LE. Prospective study of the spontaneous course of subclinical hypothyroidism: prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. Journal of Clinical Endocrinology & Metabolism. 2002 Jul 1; 87(7):3221–3226. [https://doi.org/10.1210/jcem.87.7.8678]
- Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010 Sep 22; 304(12):1365–1374. [https://doi.org/10.1001/jama.2010.1361]

© 2025 BetterByDesign Nutrition Ltd. All rights reserved.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
