Introduction
News outlets highlight when someone has died of complications of COVID-19, stressing that the person “had no underlying health conditions“, but the problem is that this is often assumed, not assessed. Just because a person wasn’t diagnosed with diabetes, heart disease or high blood pressure does not mean that they have no underlying health conditions.
Not Assessed – Assumed “Fine”
We have known since 2018 that 88% of Americans are metabolically unhealthy [1], which means that only 12% of adults are metabolically healthy. An adult dying with “no underlying health conditions” may simply mean they hadn’t been assessed. Measures of metabolic health include:
- Waist Circumference: < 102 cm (40 inches) for men and 88 cm (34.5 inches) in women
- Systolic Blood Pressure: < 120 mmHG
- Diastolic Blood Pressure: < 80 mmHG
- Glucose: < 5.5 mmol/L (100 mg/dL)
- HbA1c: < 5.7%
- Triglycerides: < 1.7 mmol/l (< 150 mg/dL)
- HDL cholesterol: ≥ 1.00 mmol/L (≥ 40 mg/dL) in men and ≥ 1.30 mmol/L (50 mg/dl) in women
If a person hasn’t had their waist circumference, blood sugar or pressure, or cholesterol assessed, then they are assumed to have no underlying health conditions. Not measuring it doesn’t mean it doesn’t exist.
Tested and Everything is “Fine”
Adults may be screened for risk of becoming diabetic using a fasting blood glucose test. In a fasting blood glucose test, we only know what happens when fasting—but if we don’t know what happens between 30 and 60 minutes after consuming a carbohydrate load, we simply don’t know the full risk. An HbA1C test provides an average but still misses people who have normal blood sugar at fasting yet spike significantly after eating.
A 2-hour Oral Glucose Tolerance Test (OGTT) is considered the best way to determine risk, but it will completely miss those who spike between 30 and 60 minutes because it doesn’t measure it. We know from research that higher glucose peaks at 30-60 minutes are signs of insulin resistance [2].
The Predictor: 1-Hour Blood Glucose
Research shows that a blood sugar spike >8.6 mmol/l (155 mg/dl) one-hour after a carbohydrate load is a better predictor of future diabetes and cardiovascular death than a 2-hour reading [3]. If it isn’t assessed, we simply don’t know.
Not Tested – Not Fine
A large-scale study found that while many had normal 2-hour blood sugar results, 75% had abnormal blood sugar results between 30 minutes and 60 minutes [4]. We can’t assume health without assessment.
Three Quarters of Adults Overweight or Obese
New NHANES data indicates that more than 73% of US adults are either overweight or obese [5]. Rates of obesity are skyrocketing.
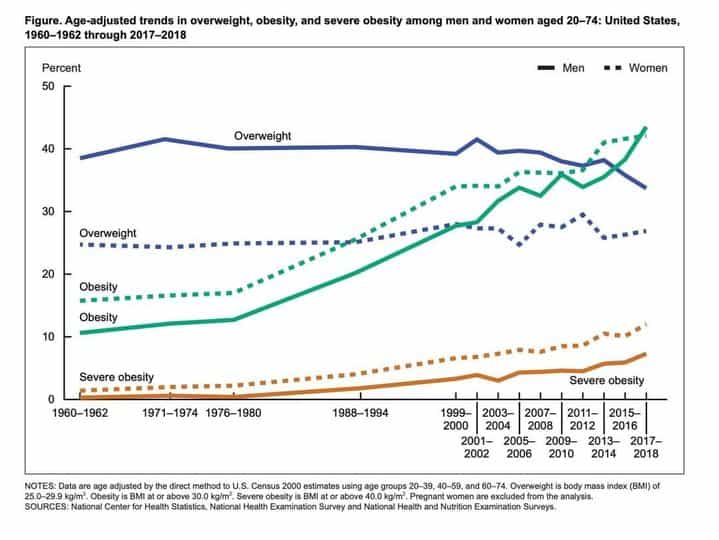
from Fryar C, et al “Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960—1962 through 2017—2018” NCHS Health E-Stats; 2020
Almost three-quarters of US adults are overweight or obese, but BMI does not assess metabolic health. BMI doesn’t tell us the whole story. Those who are overweight often have high waist circumferences [1], high blood pressure, and high fasting glucose, placing them in the metabolically unhealthy category.
Final Thoughts
America is a nation with underlying health conditions; only 12% of adults are metabolically healthy. Until we realize that we are “sick”, getting “well” is simply not possible.
More Info?
You can learn about me here.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- Araújo J, Cai J, Stevens J. Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009–2016. Metab Syndr Relat Disord. 2019 Feb;17(1):46-52. [https://doi.org/10.1089/met.2018.0105]
- Hulman A, Simmons RK, Vistisen D, et al. Heterogeneity in glucose response curves during an oral glucose tolerance test and associated cardiometabolic risk. Endocrine. 2017 Feb;55(2):427-434. [https://doi.org/10.1007/s12020-016-1126-z]
- Pareek M, Bhatt DL, Nielsen ML, et al. Enhanced Predictive Capability of a 1-Hour Oral Glucose Tolerance Test: A Prospective Population-Based Cohort Study. Diabetes Care. 2018 Jan;41(1):171-177. [https://doi.org/10.2337/dc17-1351]
- Crofts C, Zinn C, Wheldon MC, et al. Identifying hyperinsulinaemia in the absence of impaired glucose tolerance: An examination of the Kraft database. Diabetes Res Clin Pract. 2016 Aug;118:50-7. [https://doi.org/10.1016/j.diabres.2016.06.007]
- Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–2018. NCHS Health E-Stats. 2020. [https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult-17-18.htm]

© 2025 BetterByDesign Nutrition Ltd.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
