Note: This article was originally posted on July 14, 2022, and was completely updated and reposted on November 3, 2025.
Introduction
When people have blood tests to “check their thyroid,” the test that is performed is a TSH test. TSH is a pituitary hormone, not a thyroid hormone. Provincial guidelines have established that even if TSH comes back in the high-normal range, no testing of thyroid hormones is performed (i.e., no testing of free T4 or free T3) — unless the person meets the criteria that warrant a closer look.
This article covers everything you need to know about hypothyroidism, including common causes of an underactive thyroid, typical signs and symptoms associated with hypothyroidism, and outlines the various options available for having thyroid hormone blood tests done.
The Thyroid Gland
The thyroid is a butterfly-shaped gland located in the middle of the lower front part of the neck. While small, it plays a critical role in regulating metabolism—the process by which the body converts food into energy (2).
When the thyroid is underactive (hypothyroid), metabolism slows. This can affect heart rate, heat production, muscle function, thinking, and information processing (1).
The Two Main Thyroid Hormones – T4 and T3
The thyroid produces two main hormones: thyroxine (T4) and triiodothyronine (T3). About 80–90% of thyroid hormone is T4, and 10–20% is T3, most of which is converted from T4 in body tissues (6). On average, the thyroid produces roughly 85 mcg of T4 and 6.5 mcg of T3 per day—a T4:T3 ratio of about 13:1 (1).
T4 is inactive until converted to T3, the active form. In its free form, thyroxine is called free T4 (fT4), and triiodothyronine is called free T3 (fT3) (1).
T4 and T3 production is regulated by the pituitary gland, which responds to the hypothalamus. The hypothalamus releases Thyrotropin-Releasing Hormone (TRH), prompting the pituitary to release TSH (Thyroid Stimulating Hormone), signaling the thyroid to produce hormones (6).
Hypothyroidism – How it is Diagnosed
In Canada and many parts of the U.S., TSH is the standard screening test for thyroid function. If symptoms are present or TSH is high-normal, doctors may also check free T4 (7).
Central hypothyroidism occurs when the hypothalamus or pituitary gland fails to signal the thyroid gland properly. Lab tests reveal low TSH and low free T4 levels. Primary hypothyroidism occurs when the thyroid itself is underactive. Diagnosis is based on high TSH with normal or low free T4 (1).
Hypothyroidism – Main Causes
Hashimoto’s disease is the most common cause of primary hypothyroidism in developed countries. It is an autoimmune disorder producing antibodies against the thyroid, including TPO-ab and TG-ab (3). Iodine deficiency can also underlie hypothyroidism and is more common in developing countries. Other causes include thyroid surgery or radioactive iodine treatment for hyperthyroidism (1, 2).
Hypothyroidism – Getting Tested and Diagnosed
In British Columbia, unless a person is of advanced age, has a personal or family history of thyroid or autoimmune disorders, or takes medications such as lithium or amiodarone, TSH testing is only covered by MSP if the person has symptoms listed in Table 1 below (4).
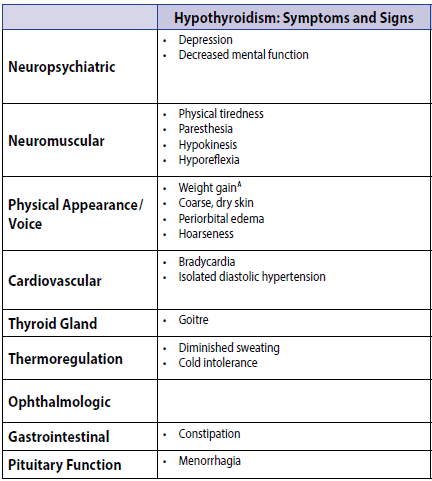
Table 1: Signs and Symptoms of Hypothyroidism (from [4])
One limitation of the checklist is that it does not include well-documented symptoms such as non-pitting edema in the lower legs, a puffy face, an enlarged tongue, loss of the outer third of the eyebrows, or pale/blue lips.
Even if TSH is tested and comes back in the high-normal range, further testing is not done (4). In order to have TSH, free T4, and free T3 tests done, the doctor needs to write them on the requisition manually.
Downloadable Checklist of Common Hypothyroid Symptoms
To support a more informed discussion with a healthcare provider, below is the link to a downloadable, fillable checklist of common hypothyroid symptoms. Keep in mind that these symptoms are not exclusive to hypothyroidism. This checklist is not intended for self-diagnosis. Only a licensed medical professional can diagnose and treat hypothyroidism.
![]() Signs and Symptoms of Hypothyroidism – Downloadable Checklist
Signs and Symptoms of Hypothyroidism – Downloadable Checklist
Thyroid Panel Lab Tests – 3 Options
1. Medical Doctor (MD)
Testing costs are generally covered by the provincial health plan if the requisition follows provincial guidelines. In Ontario, tests are outlined in the Schedule of Benefits for Laboratory Services (March 3, 2025). In BC, guidelines conform to the BC Guidelines & Protocols Advisory Committee, 2018 (5).
Provincial Lab Coverage (British Columbia – Revised March 31, 2025):
- TSH: $9.90
- Free T4: $12.12
- Free T3: $9.35
- TPO-ab: $20.22
- TG-ab: $27.90
- Reverse T3: not covered by MSP
2. Naturopathic Doctor (ND)
Thyroid assessment panels typically require out-of-pocket payment for both visits and tests. In BC, initial visits range $200–$300, while in Alberta, initial visits typically start at $325. Thyroid testing costs range from $225–$330+, plus visit costs.
3. Patient-Pay
In BC, if a doctor does not want to risk audit, they can indicate tests as “patient-pay.” The individual pays for those tests at the lab. A patient-pay price list exists for healthcare professionals titled British Columbia Private Price List for Commonly Ordered Lab Tests (April 2021).

Final Thoughts
Determining whether your symptoms are related to your thyroid can be challenging. I hope the information in this article helps you have an informed discussion with your doctor.
More Info
As you can read about under the About Me tab, I will advocate for clients who have symptoms that may be consistent with hypothyroidism or subclinical hypothyroidism to obtain adequate testing to rule out a diagnosis or enable a doctor to make one. You can learn about the Hypothyroid Management Package here.
To your good health!
Joy
Follow Me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid. 2014 Dec 1;24(12):1670–1751. [https://pubmed.ncbi.nlm.nih.gov/25266247/]
- Berkow R, Beers MH, Fletcher AJ. The Merck Manual of Medical Information. Whitehouse Station, N.J.: Merck Research Laboratories; 1997. [https://cmc.marmot.org/Record/.b10805436]
- Puszkarz I, Guty E, Stefaniak I, Bonarek A. Role of food and nutrition in pathogenesis and prevention of Hashimoto’s thyroiditis. 2018. [https://doi.org/10.5281/zenodo.1320419]
- BC Guidelines & Protocols Advisory Committee. Thyroid Function Testing in the Diagnosis and Monitoring of Thyroid Function Disorder. October 24, 2018. [https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/thyroid-function-testing.pdf]
- Laboratory Services Act. Laboratory Service Regulation. October 1, 2015 (last amended March 31, 2025 by B.C. Reg. 52/2015). [https://www.bclaws.gov.bc.ca/civix/document/id/crbc/crbc/52_2015]
- NCBI Bookshelf. Physiology of thyroid hormones. 2023. Available at: [https://www.ncbi.nlm.nih.gov/books/NBK499850/]
- Canadian Thyroid Association. Thyroid Testing Guidelines. 2023. Available at: [https://www.thyroid.ca/thyroid-testing-guidelines/]
- World Health Organization. Iodine Deficiency Disorders. 2024. Available at: [https://www.who.int/news-room/fact-sheets/detail/iodine-deficiency-disorders]
- Government of British Columbia, Ministry of Health. Schedule of Fees for Laboratory Services – Outpatient, Payment Schedule. [Revised March 31, 2025]. [https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/medical-services-plan/laboratory_services_schedule_of_fees.pdf]
- Ministry of Health Ontario. Schedule of Benefits for Laboratory Services (SOB‑LS). February 14, 2025 (effective March 3, 2025). [https://www.ontario.ca/files/2025-03/moh-ohip-schedule-of-benefits-laboratory-services-2025-03-03.pdf]

© 2025 BetterByDesign Nutrition Ltd. All rights reserved.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
