[This article was written on November 10, 2024, and was updated on October 10, 2025.]
Introduction
We are finally breaking the stigma and talking about mental health. Men grow moustaches in November to raise awareness about prostate health, so it is time to move past embarrassment and talk about colorectal health. This is my first article in this area and is about ways to reduce the incidence of painful conditions related to hemorrhoids. An article related to alcohol consumption as a risk factor for colon or rectal cancer is next.
What are Hemorrhoids?
The most well-known type of hemorrhoids, sometimes called “piles,” are swollen, inflamed veins (like varicose veins) in the rectum, or on the anus that can be painful, itchy, and may bleed, and are frequently (pardon the pun) the butt of jokes. These are external hemorrhoids that form under the skin around the anus and may resolve with a few days of over-the-counter ointment, but can become enlarged and painful.
Internal hemorrhoids are located on the lining of the rectum above what is called the dentate line (2-4 cm / 3/4 – 1.5 inches from the opening of the anus). These are normal structures that are aligned in three columns in the rectum and function like bubble wrap — cushioning the rectum against irritation from the stool until a bowel movement [1].
Most people are unaware that internal hemorrhoids are there until one becomes irritated and swollen, or worse, prolapses and protrudes from the anus. Internal hemorrhoids may result in chronic, low-grade internal bleeding can indeed lead to iron deficiency or iron-deficient anemia, even when people have no idea they are losing blood.
There are four grades of internal hemorrhoids based on the degree of prolapse.
Grade 1: Not at all prolapsed.
Grade 2: Prolapses with a bowel movement, but retracts by itself.
Grade 3: Prolapses with a bowel movement and has to be manually pushed it back in.
Grade 4: Prolapsed but can’t be pushed back in, or only with a lot of pain.
Since internal hemorrhoids lie above the dentate line, they don’t have nerve endings, and are painless and remain that way until one becomes irritated — or worse, becomes inflamed and protrudes from the rectum like a large, angry grape.
If an inflamed internal hemorrhoid is located on the left lateral side, it may be too painful to sleep on that side, and if it is located on the right posterior side, it may be too painful to sleep on one’s back. Regardless of where it’s located, a Grade 3 or 4 hemorrhoid may make it too uncomfortable to sleep much at all — and since people are generally too embarrassed to talk about hemorrhoids, this pain is largely endured in silence.
Note: external hemorrhoids that lie at the dentate line are internally located but are considered external hemorrhoids because they are at or below the dentate line. These have many nerve endings and, once inflamed, can also prolapse outside the anus. If they don’t resolve with over-the-counter treatment, surgical procedures to remove them are required.
A blood clot may form within a hemorrhoid, causing it to become thrombosed, and if this causes the blood supply to get cut off, a strangulated hemorrhoid results, which is excruciatingly painful.
The pain of hemorrhoids ranges considerably. It’s only once an internal hemorrhoid becomes irritated, swollen, and inflamed that it becomes painful. If an internal hemorrhoid or an external hemorrhoid at the dentate line prolapses, the pain can go from a 1-3 on a Likert pain scale of 1- 10 (with 10 being the worst) to an 8 or 9 on 10, and this can occur suddenly, without warning. A person can literally go from having no awareness of having internal hemorrhoids or external hemorrhoids at the dentate line, to having a prolapsed hemorrhoid, and significant pain.
Treatment for Hemorrhoids
Internal hemorrhoids above the dentate line can be treated with rubber band ligation (RBL), which is the most common first-line treatment [2, 3]. This is where a small rubber band is applied to the base of the hemorrhoid and cuts off the blood supply to it. In essence, this is a planned strangulated hemorrhoid. Over a week or two (depending on the hemorrhoid’s size), the walls will thicken, and the overall size of it will shrink. After approximately 10-14 days, the rubber bands fall off the hemorrhoid, leaving an ulcer. The ulcer may bleed slightly with bowel movements over a few days as it heals [4]. Finally, what will remain is a bit of scar tissue on the rectal wall, and that may continue to bleed lightly during bowel movements until it heals completely over the following few weeks. While the banding procedure itself is painless when done properly, and is usually performed without anesthesia, the pain from the hemorrhoid itself can be significant until it finally falls off after ligation, and heals. If banding doesn’t work or if the hemorrhoid becomes inflamed or prolapsed, surgery will likely be required.
In some cases, after hemorrhoid banding, or after an external hemorrhoid at the dentate line gets better on its own, a rectal polyp may form from the ulcer that remains where the hemorrhoid was. In some cases, the polyp can become larger than the original hemorrhoid and may become inflamed and prolapse out of the anus. Since rectal polyps can form for reasons other than a previously existing hemorrhoid, surgery will be recommended to remove the polyp, and a biopsy will be performed to determine if the polyp is benign (not cancerous) or pre-cancerous.
Causes of Hemorrhoids
Hemorrhoids, both internal and external, were previously thought to be preventable mainly through dietary changes; yet diet is only part of reducing the likelihood of getting hemorrhoids. More than two-thirds of Canadians and Americans engage in a daily habit that significantly increases the risk of developing hemorrhoids, and simple lifestyle changes can help reduce that risk.
Half of adults will have had hemorrhoids by age fifty, yet it’s rare for people to talk about them. Only 4% of people go to their doctor for help because they’re embarrassed, and the last thing they want is to have someone have a look “down there” and poking around. They just want their hemorrhoids to stop hurting and to go away— and the faster, the better. Most people will self-treat with Epsom salt sitz baths and over-the-counter topical creams or wipes, and only seek medical help if the symptoms persist or get worse.
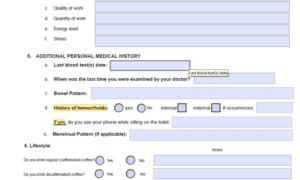 As a Dietitian, I have routinely asked my clients about their bowel function, including how often they poop and its texture — and most are fine with answering these questions because they know this is within my scope of practice. Even though I was taught that part of what can help people avoid hemorrhoids is dietary, until recently, I never asked anyone whether they’ve been experiencing hemorrhoids. This has changed. While getting enough of the right type of fiber and drinking sufficient water are important, two lifestyle factors are thought to contribute to the development of hemorrhoids, and these are the focus of this article.
As a Dietitian, I have routinely asked my clients about their bowel function, including how often they poop and its texture — and most are fine with answering these questions because they know this is within my scope of practice. Even though I was taught that part of what can help people avoid hemorrhoids is dietary, until recently, I never asked anyone whether they’ve been experiencing hemorrhoids. This has changed. While getting enough of the right type of fiber and drinking sufficient water are important, two lifestyle factors are thought to contribute to the development of hemorrhoids, and these are the focus of this article.
The good news is that by adopting a few simple dietary changes and modifying two lifestyle habits, the risk of developing hemorrhoids can be reduced.
Most people know that avoiding constipation is important to reduce the risk of getting hemorrhoids, and think that drinking enough water and eating lots of “roughage” is the way to accomplish that. What few realize is that some types of fiber can make constipation worse — especially if there is insufficient water intake. But reducing the risk of hemorrhoids involves more than diet. The length of time that we sit on the toilet, as well as the position that we sit on it, both play a significant role in the risk of developing hemorrhoids.
Squatting versus Sitting Toilet
In much of Asia, South East Asia, and Africa, the squatting toilet is the norm. The user positions themselves in a squat position over a floor-level porcelain bowl, which results in the colon and rectum being positioned in a straight line. This enables bowel movement to occur significantly faster and without straining than what occurs when using a western-style pedestal toilet. These are more than “holes in the ground” but are real toilets with a flush mechanism that the user engages to empty the bowl — just like on a Western toilet.
In Europe and most of the West, the pedestal toilet is the norm, which is used in a sitting position. This type of toilet results in a bend in the alignment between the colon and the rectum, causing it to take longer to have a bowel movement, and frequently requiring more than one “visit” to accomplish it. Of importance, the seat design of a pedestal toilet results in increased pressure on the rectum and anus, which significantly increases the risk of developing hemorrhoids.
Middle Eastern and North African countries have both squatting and pedestal toilets, depending on the region.
There are various types of squatting platforms available for purchase that can be placed over a standard Western pedestal toilet, converting it into a squatting toilet. These are popular with people who have emigrated from countries where squatting toilets are the norm.
Also available online are various types of squatting footstools that are placed in front of a standard Western pedestal toilet and enable the user to sit in a semi-squatting position. These squatting stools allow for better alignment of the colon and the rectum, and are frequently recommended to people recovering from hemorrhoids, hemorrhoid ligation (banding), and hemorrhoid surgery. These squatting stools allow for less pressure on the anus and pelvic floor, and as a result, may help reduce the development of hemorrhoids or deterioration of unknown internal hemorrhoids.
The Length of Time Sitting on a Pedestal Toilet
Due to the shape of the seat on a Western-style pedestal toilet, the length of time that one sits on it increases the risk of developing hemorrhoids. This is due to the increased pressure on the pelvic floor, lower rectum, and anus resulting from the seat’s shape.
Think of a single-hole paper punch.
 The pressure exerted over a small hole is what makes a one-hole paper punch so effective. Good for paper, not good for rectums.
The pressure exerted over a small hole is what makes a one-hole paper punch so effective. Good for paper, not good for rectums.
To limit pressure on the rectum and anus, it is recommended to limit “seat time” to 3-5 minutes at a time, 10 minutes maximum in 24 hours [1].
Washrooms as Phonebooths
In the early 1950s, most houses only had one washroom or bathroom, so multiple members of the same household had to do what they needed to in a limited time and get out. It was rare to have the luxury of being able to sit on the toilet for an extended period of time, reading the newspaper. Now, 97% of new home construction has more than one washroom or bathroom [5] — most often having two full washrooms, plus an additional 1/2 bathroom containing a toilet and a sink.
 With three toilets per house for an average family size of three in Canada [6] means that each member of the average household has access to a toilet on demand, and can — and does spend inordinate amounts of time sitting on it.
With three toilets per house for an average family size of three in Canada [6] means that each member of the average household has access to a toilet on demand, and can — and does spend inordinate amounts of time sitting on it.
A recent study found that 2/3 of Canadians and even more Americans are on their smartphones while sitting on the toilet [6]. The washroom is the new phone booth. It is one of the only places in the house where some can have time alone, and all this increased sitting on the toilet scrolling on the phone is thought to be related to the increased rates of hemorrhoids seen in younger and younger adults.
Final Thoughts
There are simple things we can do to lower the risk of developing hemorrhoids.
We can drink more water and eat enough of the right types of fibre.
A squatting stool can help align our colon, making defecation time shorter, while reducing the amount of pressure on our rectum.
It is recommended to limit “seat time” to 3-5 minutes. Not scrolling on the phone while sitting on the toilet will make it possible to do what is needed in the recommended amount of time, significantly reducing the risk of developing hemorrhoids.
Remembering how a one-hole punch works may be a helpful reminder.
For those who have never experienced the pain of a large, prolapsed hemorrhoid, implementing these changes may help avoid the experience. For those who have, I hope that learning how to minimize the risk of another will be welcomed news.
More Info
If you have been struggling with hemorrhoids but have been too embarrassed to get help, this is a topic I discuss with all my clients and am quite comfortable doing so. Learn about me and the support I can provide through the Comprehensive Dietary Package.
To your good health.
Joy
You can follow me on:
Twitter: https://twitter.com/jyerdile
Facebook: https://www.facebook.com/BetterByDesignNutrition/
References
- UT Southwestern Medical Centre, Treating hemorrhoidal disease: Conservative vs. surgical approaches, April 14, https://utswmed.org/medblog/best-ways-to-treat-hemorrhoids/
- Zagriadskiĭ EA, Bogomazov AM, Golovko EB. Conservative Treatment of Hemorrhoids: Results of an Observational Multicenter Study. Adv Ther. 2018 Nov;35(11):1979-1992. doi: 10.1007/s12325-018-0794-x. Epub 2018 Oct 1. Erratum in: Adv Ther. 2018 Nov;35(11):1993. doi: 10.1007/s12325-018-0817-7. PMID: 30276625; PMCID: PMC6223991. https://pmc.ncbi.nlm.nih.gov/articles/PMC6223991/
- McKeown DG, Goldstein S. Hemorrhoid Banding. [Updated 2024 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558967/
- Hawkins AT, Davis BR, Bhama AR, Fang SH, Dawes AJ, Feingold DL, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum. 2024 May 1. 67 (5):614-623. https://pubmed.ncbi.nlm.nih.gov/38294832/
- Eye on Housing, Number of Bathrooms in New Homes in 2021, November 3, 2022, https://eyeonhousing.org/2022/11/number-of-bathrooms-in-new-homes-in-2021/
- Statistics Canada, Average Family Size in Canada, 2021 https://www.statista.com/statistics/478948/average-family-size-in-canada/
- Toronto Sun, Two-thirds of Canadians take smart phones into the bathroom: Survey, May 16, 2022, https://torontosun.com/news/national/survey-65-of-canadians-take-their-smart-phones-into-the-bathroom

© 2025 BetterByDesign Nutrition Ltd.

Joy is a Registered Dietitian Nutritionist and owner of BetterByDesign Nutrition Ltd. She has a postgraduate degree in Human Nutrition, is a published mental health nutrition researcher, and has been supporting clients’ needs since 2008. Joy is licensed in BC, Alberta, and Ontario, and her areas of expertise range from routine health, chronic disease management, and digestive health to therapeutic diets. Joy is passionate about helping people feel better and believes that Nutrition is BetterByDesign©.
