Several recent studies have found a relationship between the species of bacteria and fungi that live in our large intestine, carbohydrate intake and Irritable Bowel Disease (IBD), including Ulcerative Colitis and Crohn’s disease. This article elaborates on how this knowledge may help improve symptoms for those with IBD.
The Gut Microbiome & Mycobiome
The trillions of gut bacteria that live in our intestines are collectively referred to as the ‘gut microbiome, ‘gut microbiota’ or ‘gut flora’, along with fungi (called the ‘mycobiome’) and other single cell organisms called archaea.
We are in a symbiotic relationship with these gut bacteria — which means when things are going well, they benefit us and we benefit them. What we eat feeds them, and in turn they produce by-products that are helpful for us. One example of a helpful end-product of fermentation by the so-called “good bugs” of our gut microbiome is the formation of short chain fatty acids (SCFA) [3], which plays an important role in maintaining glucose (blood sugar) levels, fat metabolism and even appetite regulation [2] in humans. As I will elaborate further on in this article, these SCFA also play a role in keeping the “bad bugs” from taking over.
The gut mycobiome, which are the species of fungi that live in our large intestine can have an impact on our gut microbiome, and both are affected by the carbohydrates we take in through the diet — which has important implications for those with Inflammatory Bowel Disease.
Dietary Carbohydrate
What types of foods are carbohydrate-based may seem obvious to some, but many people don’t realize that simple sugars such as glucose (the sugar in our blood) and fructose (the sugar in fruit) are not that much different than ‘starches’, such as bread, pasta and rice. As outlined in a previous article, sugars can come alone come alone, in pairs or strung like pearls on a chain. Knowing the different types of sugars is important to those with Inflammatory Bowel Disease as these sugars and starches can be used as food for our gut microbiome, and which bacteria and fungi we ‘feed’ has important implications on health.
Simple Sugars – monosaccharides & disaccharides
Simple sugars can come alone (monosaccharides, which means ‘one sugar’) or in pairs (disaccharides, which means ‘two sugars’).
Monosaccharides include glucose, fructose and galactose and disaccharides are combinations of these monosaccharides linked together, in pairs. Some common disaccharides include sucrose, lactose and maltose;
Sucrose is ordinary table sugar and made up of glucose-fructose.
Lactose is the sugar in milk and milk products and is made from a glucose-galactose pair.
Maltose which rarely occurs naturally in foods, is glucose-glucose. Maltose is used in food processing such as the shiny glaze on Chinese roast duck.
Complex Carbohydrates – strings of sugar molecules
Complex carbohydrates are made up of more than two monosaccharides (sugar molecules). Oligosaccharides (‘oligo’ means ”scant” or ”few”) are made up of 3-10 sugar molecules, whereas polysaccharides (including starch) are made up of hundred or even thousands of monosaccharides (sugar molecules).
Oligosaccharides
Oligosaccharides are made up of 3-10 sugar molecules and the two most common are some of the complex carbohydrates found in dried beans, peas and lentils[1]. For example, raffinose is an oligosaccharide made from 3 sugar molecules: galactose-glucose-fructose and stachyose is an oligosaccharide made from 4 sugar molecules: galactose-galactose-glucose-fructose. What is important to know is that the body can’t break down either raffinose or stachyose, but these are fermented by certain species of bacteria in our gut microbiome.
Polysaccharides
Polysaccharides are made up of hundreds or thousands of sugar molecules linked together. When those sugar molecules are only glucose, the polysaccharide is called ”starch”.
Some polysaccharides form long straight chains while others are branched like a tree. These structural difference affect how these carbohydrates behave when they’re heated or put in water. The way the monosaccharides are linked together makes the polysaccharides either digestible as in starch, or indigestible as in fiber.
We can’t digest polysaccharides found in plant foods such as fiber, cellulose, hemicellulose, gums and mucilages (such as psyllium) but they can both slow down the absorption of digestible carbohydrate and be fermented by the gut microbiome.
Starch
Starches are long chains of glucose molecules strung together like beads on a string. Starches are found in grains such as wheat, corn, rice, oats, millet and barley, as well as in legumes such as peas, beans and lentils* and tubers such as potatoes, yams and cassava.
*As mentioned above, peas, beans and lentils also have the complex carbohydrates called oligosaccharides which are not broken down by the body, but are broken down by bacteria in our gut microbiome.
There are two types of starches; the long unbranched chains called amylose and the long branched chain ones call amylopectin. The body digests most starches very easily, although those with a high percentage of amylopectin (such as cornstarch) are digested much more easily than those with a high amount of amylose, such as wheat starch [1].
Since starches are just glucose molecules linked together and they are easily broken down to individual glucose molecules, so starches quickly affect the blood sugar and as I will elaborate on in this article are fermented easily by our gut microbiome and may play a role in colitis in genetically susceptible individuals. Limiting these and other fermentable carbohydrates also can play a role in reducing symptoms of those with IBD.
How Simple Sugars can Induce Colitis by Affecting the Microbiome
A study was published in late 2020 documenting how simple sugars in the diet can induce colitis, an inflammatory bowel disease [2]. The study found that when researchers fed mice simple sugars such as glucose, fructose and sucrose, the high-sugar diet damaged the protective mucus layer of the colon (large intestine) and increased the number of harmful bacteria — especially Akkermansia muciniphila and Bacteroides fragilis which break down the mucus that lines and protects the colon.
The study found that when the mice were fed a 10% glucose solution for seven days (chosen because soft drinks contain ~15% sugar) and were then given a 2.5% dextran sulfate sodium (DSS) which is known to induce colitis, the mice that had been fed the glucose had extreme sensitivity to DSS treatment and suffered from aggressive colitis, bloody diarrhea and rapid loss of nearly 20% of their body weight. When the researchers looked at the glucose-treated mice three days after giving them the DSS, they found that their colons were shorter than the colons of the control mice that were not fed the glucose, and that the glucose-fed mice had many of the symptoms of colitis, including loss of epithelial crypts, inflammation, and ulceration.
When the researchers saw that the high-sugar intake made the colitis
caused by DSS chemical injury of the colon worse, it led them to then test
whether high sugar intake alone had a similar effect in mice that were genetically susceptible. They treated mice with genetic susceptibility to colitis with a 5% glucose solution from 14 weeks of age, while measuring weekly body weight changes and clinical scorings for 5 weeks. At 19 weeks, 90% of glucose-treated genetically-susceptible mice developed colitis, compared to 40% in the controls that did not have the genetic susceptibility. The glucose-fed susceptible mice had much greater loss of body weight and higher diarrhea and rectal bleeding compared to control the control mice, and when they looked at the colon tissue of the mice, the ones that were glucose-fed had increased inflammation. There was also a much higher expression of inflammatory molecules in the colons of sugar-treated mice.
Of Mice and Men
Even though the results of animal studies can’t be applied directly to humans, this study can give us an indication of what may be going on in people.
The National Human Genome Research Institute explains it this way;
“Mice and humans share virtually the same set of genes. Almost every gene found in one species so far has been found in a closely related form in the other. Of the approximately 4,000 genes that have been studied, less than 10 are found in one species but not in the other” [3].
Low-FODMAP Diet in Inflammatory Bowel Disease – effect on microbiome
For people with Inflammatory Bowel Disease, including Crohn’s disease and Ulcerative Colitis, a low-FODMAP diet is successfully used to reduce symptoms of the disease once their symptoms have been stabilized using a low residue diet after a flare. A low-FODMAP diet enables people with IBD to gradually normalize their diet, while avoiding foods that can be fermented by the ‘gut microbiome’ and this often leads to those with IBD finding significant relief of symptoms.
FODMAP is an acronym for fermentable, oligo-, di-, monosaccharides and polyols. A low-FODMAP diet reduces foods which contain various sugars such as fructose (the sugar found in fruit), lactose (the sugar in milk), sugar alcohols called ‘polyols’ such as sorbitol and mannitol, fructans which are found in garlic, leeks, artichokes, and wheat, and galacto-oligosaccharides which are found in legumes such as lentils, chickpeas, and black beans. As outlined above, these FODMAPS are fermentable by the gut bacteria and the by-products of that fermentation have long been thought to underlie symptoms experienced in those with Inflammatory Bowel Disease (IBD), as well as Irritable Bowel Syndrome (IBS).
Over the last 5 years since I began using a therapeutic low carbohydrate diet to reduce the symptoms of type 2 diabetes and for weight loss, I began to wonder if what made a low-FODMAP diet effective in reducing symptoms in IBD was due to its overall low-carbohydrate content — not just the lower amount of fermentable, oligo-, di-, monosaccharides and polyols. Two studies published towards the end of 2020 confirmed a relationship between other types of carbohydrate in the diet and the gut microbiome (bacteria) and mycobiome (fungi). The first study was about the relationship between simple sugars intake and colitis which is outlined above, and the second study was about the effect of a very low carbohydrate diet on species of gut fungi (mycobiome), and is outline below.
Very Low Carbohydrate Diet Reduces Some Fungi in Gut Microbiome
Shortly before the above study showing a relationship between simple sugar intake and colitis is genetically-susceptible mice was published, there was another study that looked at the effect of a Mediterranean ketogenic diet* to decrease the population of certain species of gut fungi (mycobiome) that populate the gut, along with the bacteria (microbiome).
*A ketogenic diet is one that is very low in dietary carbohydrates — usually less than 20 grams of carbohydrate per day.
While it was a small pilot study, it was a randomized, double-blind crossover study which is the strongest study design. This type of study has two groups of people that don’t know which of the two groups they are in and who received one diet for half the study period, and then the diets and groups are switched so they receive the other diet for the second half of the study.
This study looked at the effect of Mediterranean Ketogenic Diet (MMKD) compared to the American Heart Association Diet (AHAD) in people with mild cognitive impairment (MCI) and found that symptoms of MCI were improved with the Mediterranean Ketogenic Diet in relationship with changes in the gut mycobiome.
What researches found was that (1) whether a person had Mild Cognitive Impairment or not, the Mediterranean Ketogenic Diet more positively affected the gut mycobiome than the AHAD diet and (2) in those with MCI, there was a significant reduction in the proportion of Candida species during the Mediterranean Ketogenic Diet phase.
It was this part of the discussion that got my attention in relationship to Irritable Bowel Disease, such as Crohn’s disease and Ulcerative Colitis.
“The genus Candida comprises many opportunistic species implicated in various gut-related diseases including inflammatory bowel diseases, Crohn’s disease, ulcerative colitis, and gut inflammation [78]…In this context, reduced Candida carriage in patients with MCI might reflect another positive outcome of the MMKD intervention.”
What this means is, the researchers wondered whether a Mediterranean Ketogenic Diet (MMKD) might be effective in lowering Candida which has already been implicated in Inflammatory Bowel Disease, including Crohn’s disease and ulcerative colitis.
This part of the discussion section also stood out;
“Notably, we find a significantly negative correlation of Candida with short-chain fatty acid butyrate, a beneficial gut bacterial metabolite which was found to be increased by MMKD in these patients with MCI [24]. One of the ways gut bacteriome keep mycobiome in check is through the production of wide range of small molecules such as SCFAs (e.g., butyrate), which have inhibitory effects against the growth of pathobionts including Candida albicans [79, 80]. Together, these data suggest that the MMKD positively modulates the gut microbiome as well as the bacterial metabolites arrays, which in turn may check the overgrowth of opportunistic pathogens such as Candida.”
Simply said, what this means is that it is well-known that a ketogenic diet increases the amount of the short chain fatty acid (SCFA) butyrate which inhibits the growth of strains of Candida. This relationship implies a therapeutic role for a Mediterranean ketogenic diet in the management of Irritable Bowel Syndrome.
Final Thoughts
In light of the above two studies, it seems to make good sense for those at genetic risk of developing Irritable Bowel Disease — as well as for those already diagnosed with IBD to
(a) reduce intake of simple sugars, including glucose, fructose and sucrose
and
(b) consider adoption of a Mediterranean Ketogenic Diet which has been found to reduce the amount of Candida species — which has already been implicated in the development of Irritable Bowel Disease.
More Info?
If you would like more information about my services then please have a look under the tab of that name or send me a note through the Contact Me form.
To your good health!
Joy
You can follow me on:
Twitter: https://twitter.com/JoyKiddie
Facebook: https://www.facebook.com/BetterByDesignNutrition/
Copyright ©2021 BetterByDesign Nutrition Ltd.
LEGAL NOTICE: The contents of this blog, including text, images and cited statistics as well as all other material contained here (the ”content”) are for information purposes only. The content is not intended to be a substitute for professional advice, medical diagnosis and/or treatment and is not suitable for self-administration without the knowledge of your physician and regular monitoring by your physician. Do not disregard medical advice and always consult your physician with any questions you may have regarding a medical condition or before implementing anything you have read or heard in our content.
References
- Morrison DJ, Preston T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes. 2016;7(3):189-200. doi:10.1080/19490976.2015.1134082
- Khan S, Waliullah S, Godfrey V et al, Dietary simple sugars alter microbial ecology in the gut and promote colitis in mice, Science Translational Medicine 28 Oct 2020: Vol. 12, Issue 567, DOI: 10.1126/scitranslmed.aay6218
- National Human Genome Research Project, Why Mouse Matters, https://www.genome.gov/10001345/importance-of-mouse-genome
- Nagpal R, Neth B, Wang S et al, Gut mycobiome and its interaction with diet, gut bacteria and alzheimer’s disease markers in subjects with mild cognitive impairment: A pilot study. EBioMedicine, 2020; 59: 102950 DOI: 10.1016/j.ebiom.2020.102950


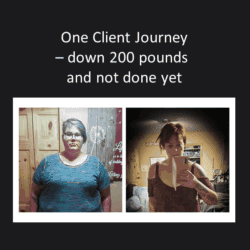

 In April 2019, Karen private messaged me on social media and sent me a photo of herself, after she had lost 150 pounds. It was both delightful and very rewarding to receive this from a client and to see that she had continued to apply what she had learned, and was doing exactly what she set out to do. She gave me permission to share it on social media with only her first name and initial of her last name, which I did. All people knew is that this was what one client had accomplished in a year.
In April 2019, Karen private messaged me on social media and sent me a photo of herself, after she had lost 150 pounds. It was both delightful and very rewarding to receive this from a client and to see that she had continued to apply what she had learned, and was doing exactly what she set out to do. She gave me permission to share it on social media with only her first name and initial of her last name, which I did. All people knew is that this was what one client had accomplished in a year. Last week instead of private messaging me an update, Karen decided to post a compilation photo of herself under one I had posted of myself on Facebook. Even though I had not spoken to her in over a year, there was her picture for everyone, including me, to see! Wow!! Karen had lost more than 200 pounds, and had every reason to be proud of her accomplishment!
Last week instead of private messaging me an update, Karen decided to post a compilation photo of herself under one I had posted of myself on Facebook. Even though I had not spoken to her in over a year, there was her picture for everyone, including me, to see! Wow!! Karen had lost more than 200 pounds, and had every reason to be proud of her accomplishment!  “I started keto on my own in January 2018, but it really stressed me out. There is so much information ‘out there’, and everything contradicted itself. It didn’t make sense to me. Macros, IF, fat bombs…..even in my coffee. Seriously, don’t mess with my coffee.
“I started keto on my own in January 2018, but it really stressed me out. There is so much information ‘out there’, and everything contradicted itself. It didn’t make sense to me. Macros, IF, fat bombs…..even in my coffee. Seriously, don’t mess with my coffee.
